
Co-authored by Vincent E. Martinelli, Jr. and Perplexity AI. See Disclosures.
Worried about cholesterol?
Here are facts and solutions.
Stop Letting
“Normal” Cholesterol
Age Your Arteries!
Decode Your LDL/HDL Ratios
Fix the Real Problem
Talk to Your Doctor Before Your Next Lab Report Arrives
Introduction
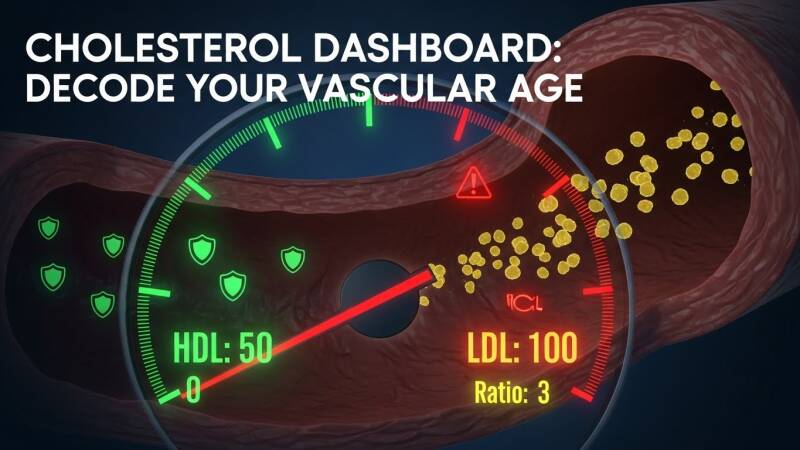
Your lipid panel is a dashboard, not a verdict: LDL pushes plaque into arteries, HDL pulls it out, ratios reveal balance, and metabolic terrain amplifies the stakes. For Americans, where 1 in 3 adults battles high cholesterol amid obesity and diabetes epidemics, understanding these numbers—LDL under 100 mg/dL optimal, Total/HDL ratio below 3 favorable—turns confusion into control, slowing vascular aging before symptoms strike.
Author’s Note
Written in a clinician's voice—precise, pattern-focused, and free of hype—this piece draws from guideline consensus (AHA/ACC 2018 and beyond), cohort studies, and preventive cardiology practice. It empowers readers to interpret labs, grasp ratios, and align lifestyle with biology, without overselling unproven levers.
Preface
Cholesterol management is not about chasing "good" versus "bad" labels but decoding the signals your arteries send about their long-term health. This article distills the science into actionable clarity for Americans navigating lipid panels amid rising cardiometabolic risks.
Cholesterol is really a story about patterns over time: how much cholesterol is being pushed into your artery walls, how much is being pulled out, and what kind of metabolic “weather” those arteries live in. Your numbers are not a moral verdict; they are a snapshot of how fast or slow your vascular system is aging.
The core panel: what each number means
When you get a standard cholesterol panel, you are really looking at several distinct (but related) markers of risk. Total cholesterol is the big headline number, but it is crude on its own; the breakdown into LDL, HDL, non‑HDL, triglycerides, and ratios is where the real story lives. LDL (low‑density lipoprotein) is the main “delivery truck” that carries cholesterol into tissues, including the artery wall, and long‑term elevation is a proven, causal driver of plaque buildup and atherosclerotic cardiovascular disease. HDL (high‑density lipoprotein) is more like the cleanup crew, involved in reverse cholesterol transport and a whole web of anti‑inflammatory, antioxidant, and endothelial effects; higher levels usually track with lower risk, although HDL behaves more like a risk marker than a lever you can reliably pull with drugs.
Triglycerides are circulating fats that tend to run high in the setting of insulin resistance, excess refined carbohydrate, excess calories, and certain genetic traits. Non‑HDL cholesterol (total cholesterol minus HDL) conveniently bundles all the “bad actors” together—the LDL and its cousins that carry apoB and can infiltrate the arterial wall—and often predicts events as well or better than LDL alone, especially when triglycerides are elevated. Total cholesterol still matters, but in modern practice it mostly serves as a starting point before zooming in on LDL, non‑HDL, and the key ratios.
What counts as “good” and “bad” numbers
For most adults without known heart or vascular disease, an LDL under 100 mg/dL is typically considered optimal, with tighter targets (often below 70 mg/dL and sometimes even lower) for people who already have coronary disease, diabetes with high risk, or evidence of plaque on imaging. HDL is generally considered adequate at 40 mg/dL or higher in men and 50 mg/dL or higher in women, with many epidemiologic curves suggesting that benefits level off somewhere in the 60–70 mg/dL range and, at very high levels, may even reverse in some subgroups. Total cholesterol below 200 mg/dL and non‑HDL below about 130 mg/dL are common population‑level goals, with more aggressive non‑HDL targets in those at higher baseline risk.
Triglycerides below 150 mg/dL are labeled “normal,” 150–199 mg/dL is borderline high, 200–499 mg/dL is high, and 500 mg/dL and above raises additional red flags for pancreatitis. These cut points, however, are just that—cut points. In real‑world practice, the interpretation is not binary. A 58‑year‑old with mildly elevated LDL, borderline triglycerides, hypertension, and a history of smoking will be viewed very differently from a 28‑year‑old with the same lipid numbers and no other risk factors. Age, blood pressure, smoking status, diabetes, kidney function, family history, and sometimes coronary calcium scoring all get folded into a 10‑year and lifetime risk estimate that guides how aggressively to intervene.
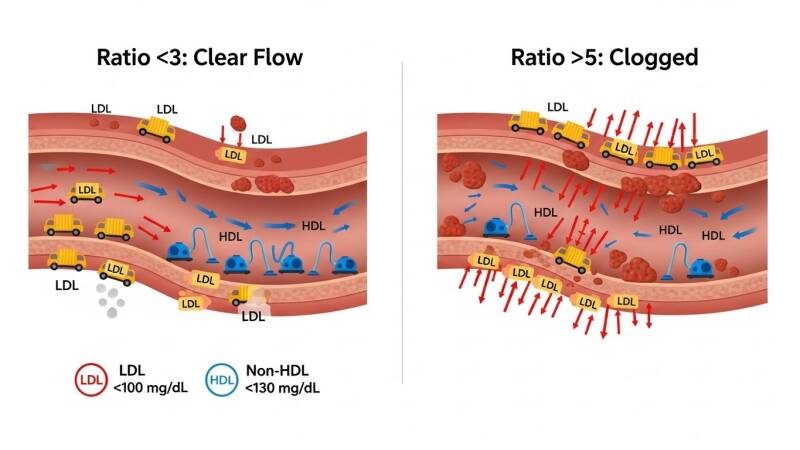
LDL, HDL, and the power of ratios
Most people have heard “LDL is bad, HDL is good,” but your arteries are more interested in balance than slogans. One simple way to visualize that balance is the total‑cholesterol‑to‑HDL ratio. This ratio compresses several moving parts into one number: the amount of cholesterol riding in potentially harmful particles versus the amount riding with the protective, cleanup particles. Many preventive cardiology clinicians treat a ratio under about 3 as a very favorable sign, while ratios drifting into the 4–5 range and beyond are associated with higher long‑term risk. It is not that the ratio replaces LDL or non‑HDL as treatment targets; rather, it gives you and your clinician a quick read on whether the overall pattern is metabolically friendly or not.
There are other ratios that sometimes appear on lab reports or in research—LDL/HDL, triglyceride/HDL, and so on. In many studies, these ratios track with insulin resistance, small dense LDL patterns, and overall cardiometabolic risk. That said, current mainstream guidelines still anchor decision‑making on absolute LDL and non‑HDL levels, the presence or absence of clinical atherosclerotic disease, and the calculated global risk score. Ratios and patterns are supporting actors that refine the picture, not standalone decision‑makers.
Beyond the number: particle quality and function
An important nuance: lipoprotein “quality” and function matter alongside the raw numbers. LDL is not a single uniform entity: there are larger, “fluffier” LDL particles and smaller, denser LDL particles. For years, small dense LDL had a reputation as uniquely dangerous, and there is evidence that these particles may bind more readily to artery walls and are more common in people with insulin resistance and metabolic syndrome. But when you adjust for the total number of apoB‑containing particles (essentially the total LDL‑like particle count), particle size fades in importance. The main issue is how many atherogenic particles are spending their days bumping into your arterial lining, not just how big they are.
HDL has its own version of this story. The laboratory number you see—HDL‑C—is just the amount of cholesterol riding inside HDL particles, not a direct measure of how well those particles can remove cholesterol from arteries or modulate inflammation. Some people walk around with decent HDL‑C but relatively “lazy” HDL function; others have modest HDL‑C but surprisingly efficient cholesterol efflux. This helps explain why drugs that substantially raised HDL‑C did not consistently reduce heart events: improving the score on paper does not guarantee better biology. In practical terms, this shifts the emphasis away from “chasing HDL” with medications and toward interventions that reliably lower apoB/LDL and improve the underlying metabolic environment in which HDL operates.
How clinicians actually use these data
In a typical visit, a clinician looks at your lipid panel through the lens of overall risk rather than in isolation. The first move is to estimate your 10‑year and lifetime risk of heart attack and stroke using age, sex, race, blood pressure, smoking status, diabetes, and sometimes kidney disease or inflammatory conditions. LDL and non‑HDL levels are then mapped onto this risk backdrop: very high LDL (for example, 190 mg/dL or higher) almost always commands attention, regardless of other factors, because it suggests a lifelong artery‑bathing insult and often hints at familial hypercholesterolemia. More modest LDL elevations may merit lifestyle changes alone in a low‑risk younger person but push a clinician toward statins or other drugs in someone older or with multiple risk factors.
The panel is also scanned for a metabolic pattern. Low HDL, high triglycerides, and only mildly elevated LDL often show up in people with central obesity, insulin resistance, and the cluster of findings called metabolic syndrome. That pattern flags not just lipid risk but also future diabetes risk and calls for a focus on weight, physical activity, sleep, blood pressure, and diet quality. Non‑HDL and total/HDL ratio add another layer: if those are substantially improved by lifestyle or medication, the clinician gains confidence that the atherogenic particle burden and overall balance have shifted in a healthier direction. Follow‑up labs then become a way of tracking whether your arteries are now “aging more slowly” on the current plan.
Lifestyle as the engine behind better numbers
Numbers change when physiology changes, and physiology changes most reliably when lifestyle does. Patterns that consistently lower LDL and non‑HDL, improve ratios, and calm the metabolic background include: eating more soluble‑fiber foods (such as oats and legumes), swapping saturated fats (from high‑fat meats and many processed foods) for unsaturated fats (from sources like nuts, seeds, olive oil, and avocado), increasing intake of vegetables and whole fruits, and limiting refined starch, added sugars, and ultra‑processed foods. Regular physical activity improves insulin sensitivity, reduces triglycerides, and tends to help HDL, while weight loss—when needed—lower LDL and triglycerides and can move the entire panel in a more favorable direction.
Inflammation, oxidative stress, and insulin resistance are the “terrain” variables that determine how toxic a given lipid profile actually is over time. Chronic stress, poor sleep, smoking or vaping, heavy alcohol use, and sedentary behavior all push that terrain in the wrong direction. On the flip side, consistent movement, restorative sleep, smoking cessation, and a minimally processed, plant‑forward diet help convert LDL and HDL from a static lab report into a more forgiving, less inflammatory environment. Add in genetics—such as familial hypercholesterolemia or other inherited lipid disorders—and you can see why two people with identical LDL numbers can have very different lifetime risks and may need very different levels of intervention.

Putting your results into a useful framework
For someone looking at a lab slip in the United States, a practical way to think about cholesterol is to turn it into a short checklist rather than a jumble of targets. First: “What is my LDL, and what goal makes sense for my risk level?” For many people, a good starting goal is under 100 mg/dL, with under 70 mg/dL (or lower) if there is known plaque, diabetes with high risk, or previous events. Second: “What are my non‑HDL and total/HDL ratio doing?” A non‑HDL under about 130 mg/dL and a total/HDL ratio under about 3 suggest that the overall balance of particles looks favorable; climbing above 4–5 on the ratio is a nudge to tighten things up. Third: “Do my triglycerides and HDL hint at insulin resistance or metabolic syndrome?” High triglycerides and low HDL are a signal to look hard at diet, weight, physical activity, and sleep.
From there, the aim is not perfection but direction. Numbers that drift slightly out of range are an invitation to sharpen lifestyle, not a reason to panic. Numbers that are clearly and persistently high—especially LDL and non‑HDL in a person with elevated risk—are a sign that medications, often starting with a statin, deserve a serious, informed conversation. All of this can be framed less as “good” versus “bad” cholesterol and more as “How fast is my arterial clock ticking, and what can be done now to slow it down?” That framing tends to reduce fear, increase agency, and align the lab report with the choices that actually change outcomes over the long arc of a life.
2025 Breakthroughs: The New Frontier in Cholesterol Control
As of late 2025, cholesterol management is entering a gene-editing era that could make lifelong pills and injections relics of the past. One-time therapies targeting PCSK9 and Lp(a)—the stubborn genetic culprits behind high LDL and inherited hypercholesterolemia—are delivering unprecedented, durable reductions, potentially slashing plaque risk without daily compliance battles.
Gene-Editing "One-and-Done" Shots
-
VERVE-102 (Verve Therapeutics): This CRISPR-based injection silences the PCSK9 gene in liver cells, boosting LDL receptors and clearing "bad" cholesterol. Early 2025 trial data in familial hypercholesterolemia patients showed LDL drops of 21–69% (average 50%+ at higher doses), sustained long-term with a single shot. No serious side effects; Phase 2/3 trials expanding globally, final results expected H2 2025. "One and done" could redefine prevention for millions.
-
CRISPR-Cas9 LDL/Triglyceride Therapy: A November 2025 NEJM pilot (15 severe cases) used CRISPR infusion to edit liver genes, yielding ~50% LDL reduction and 55% triglyceride drop at highest doses. Minimal side effects; Phase 2 starting end-2025. Targets both lipids at once, addressing the dual-threat pattern.
Lp(a) Silencers: Tackling the "Silent Killer"
Elevated Lp(a)—untreatable until now—affects 1 in 5 Americans, supercharging plaque independent of LDL. 2025 ACC highlighted:
-
Lepodisiran (Eli Lilly): siRNA therapy slashed Lp(a) by 94% for over a year with two doses (ALPACA trial). "Remarkable" for high-risk genetics; outcomes trials underway.
-
Pelacarsen and Olpasiran: Phase 3 trials (ending 2025–2026) show 80–95% Lp(a) cuts; monthly/quarterly shots. FDA watchlist for 2026 approval.
Oral and Combo Innovations
-
AZD0780 (AstraZeneca): Oral PCSK9 inhibitor matched injectables, dropping LDL 51% in 12 weeks (PURSUIT Phase 2B, ACC 2025). Pill form for statin-intolerant patients.
-
Fixed-Dose Combo (Cleveland Clinic/Lancet): New drug duo halved LDL in high-risk ASCVD, simplifying add-on therapy beyond statins.
Emerging Frontiers: Beyond Lipids to Heart Regeneration (2025 Updates)
While cholesterol control targets plaque prevention, 2025 breakthroughs are pushing into direct heart repair and novel adjuncts, offering hope for those already facing damage from decades of suboptimal LDL/non-HDL ratios. These span validated trials to preclinical innovations—none redundant with gene-editing therapies, all extending the "slow vascular aging" theme to outright reversal where possible.
Mayo Clinic Stem Cell Patch: Repairing Plaque-Damaged Hearts
Mayo Clinic researchers unveiled a minimally invasive "stem cell patch" in late 2025 preclinical trials: lab-grown heart tissue from reprogrammed adult stem cells (iPSCs) delivered via tiny chest incision, no open-heart surgery needed. The flexible, foldable patch—combining cardiomyocytes, endothelial cells, and fibroblasts on a biodegradable nano/microfiber scaffold—integrates with scarred myocardium post-infarction, boosting contractility, reducing fibrosis, spurring new vessels, and curbing inflammation in rodent models. Aligned with Mayo's Genesis Initiative, human trials could launch in 3–5 years, potentially bridging statin failures to transplant for frail heart failure patients whose arteries bore high-Lp(a)/LDL lifetimes.
Bempedoic Acid: Statin Alternative Proven in CLEAR Outcomes
The 2023 CLEAR Outcomes trial (NEJM, reaffirmed 2025 analyses) solidified bempedoic acid for statin-intolerant patients: this oral inhibitor of cholesterol synthesis cut major adverse cardiovascular events (MACE) by 13% in 14,000+ high-risk cases, with LDL drops of 20–25% and uric acid benefits. Unlike statins, it skips muscle side effects by acting in liver only—ideal for metabolic syndrome patterns (high triglycerides, low HDL). 2025 guidelines increasingly endorse it as first-line add-on or alternative, expanding options for Americans dodging polypharmacy while hitting non-HDL targets.
Magnesium as Arterial Decalcifier
Emerging 2025 reviews synthesize magnesium's role in blocking vascular calcification—a downstream hit from chronic inflammation/high LDL. Magnesium competes with calcium in soft tissues, inhibiting crystal formation and potentially resorbing deposits via osteoclast-like activity; low serum Mg correlates with accelerated atherosclerosis in cohorts. Doses of 300–400 mg/day (e.g., Mg glycinate) show promise in small RCTs for reducing coronary calcium scores alongside statins, fitting insulin-resistant terrains. Not a cure-all, but a low-risk lever for ratios plus plaque stability—monitor kidneys, as excess risks diarrhea.
Bioactive Gels and Synthetic Blood: Heart Attack Horizons
-
Bioactive Regenerative Gel: U.S. labs (e.g., Harvard-affiliated) advanced synthetic hydrogels in 2025 that mimic extracellular matrix, loaded with stem factors to regenerate infarcted tissue. Injected post-MI, they promote cardiomyocyte proliferation and angiogenesis, reducing scar size in pigs—early synergy with cholesterol control to limit damage from acute plaque rupture.
-
Synthetic Oxygen-Carrying Blood: Perfluorocarbon emulsions (no red cells needed) sustained large animals 2025 without lungs/ventilation for hours, per DARPA-funded trials. For cardiac arrest or surgery, this buys time during no-flow states, preserving myocardium until reperfusion—critical for high-Lp(a) patients prone to sudden events.

Clinician Takeaway:
Pair these with core lipid strategies: bempedoic for intolerance, Mg for calcification nudge, patches/gels as future for end-stage. Discuss with providers; trials via ClinicalTrials.gov. Your 2025 panel isn't just numbers—it's a gateway to tomorrow's resets.
These shift paradigms from symptom-chasing to root-cause editing. For FH or refractory high LDL/non-HDL, discuss trial eligibility; for average-risk Americans, they underscore urgency of baseline control (LDL<100, ratios<3) while awaiting rollout. Monitor ACC/ES 2026 for approvals—vascular aging just got a reset button.
Closing Thoughts
Cholesterol whispers your arterial future—listen via LDL, ratios, and terrain, then respond with habits that rewrite the story. Optimal patterns are earned daily, stacking odds against plaque for decades of vitality. Your next panel is feedback, not fate.
Further Reading
-
ESC/EAS Dyslipidemia Guidelines (2019)
-
Lancet: ApoB vs LDL Meta-Analysis (2023)
-
NEJM: PCSK9 Inhibitors and LDL (2024)
-
JACC: Risk-Enhancing Factors Review
-
UpToDate: Lipid Management in Primary Prevention
-
NIH: Family Heart Foundation FH Resources
-
Cleveland Clinic: Metabolic Syndrome Guide
Sources (partial list)
Important Disclosure
This article provides general educational information on cholesterol management based on established guidelines (e.g., AHA/ACC 2018 and supporting studies) and preventive cardiology principles. It is not medical advice, a diagnosis, or a treatment recommendation. Cholesterol targets, ratios, and interventions vary by individual factors including age, risk profile, genetics, and comorbidities—always consult a qualified healthcare professional for personalized interpretation of your lipid panel, risk assessment, and management plan.
No endorsements of specific products, supplements, or therapies are implied. Lifestyle suggestions (e.g., soluble fiber foods) align with broad consensus but do not replace professional guidance. The author has no conflicts of interest or financial affiliations related to pharmaceutical, nutraceutical, or dietary products discussed. Outcomes from cholesterol management depend on adherence and individual biology; past performance of interventions (e.g., statins reducing events) does not guarantee future results. Readers assume responsibility for verifying information and seeking expert care. Last updated: December 2025.
This article was crafted by Perplexity AI, an advanced language model, through extensive iterative research leveraging web searches, guideline analyses (e.g., AHA/ACC 2018 cholesterol guidelines), cohort studies, and preventive cardiology resources. Perplexity conducted comprehensive tool-based investigations into LDL/HDL targets, ratios, particle quality, metabolic context, and lifestyle impacts, synthesizing dozens of sources into the core content, structure, and refinements.
Vincent E. Martinelli, Jr., the human author, provided further research data, including and not limited to reviewing LinkedIn posts, sharing detailed research files, and source data. He also provided expert guidance, language and content editing, layout, and format input, setting the direction with a clinician's precise and pattern-focused style.
No financial conflicts exist; this is collaborative educational work.
The author of this article is not a licensed medical professional, cardiologist, or healthcare expert. This content was developed through collaborative research with AI tools, incorporating publicly available guidelines, studies, and shared resources, but it does not constitute professional medical advice, diagnosis, or treatment recommendations.
Readers must conduct their own due diligence: verify all information against current guidelines (e.g., AHA/ACC), consult qualified healthcare providers for personalized lipid interpretation, risk assessment, and management, and never rely solely on this article for health decisions. Individual results vary based on genetics, lifestyle, and comorbidities; what works for one person may not apply to another. The author assumes no liability for outcomes from applying this information. Always prioritize expert clinical guidance over general educational material. Last updated: December 2025.
This article may contain affiliate links to products from companies like LiveGood, Isagenix, Melaleuca, Young Living, doTERRA, and others. If you click on these links and make a purchase, the author may receive a commission at no additional cost to you. These commissions help support the creation of educational content like this cholesterol guide. Recommendations are based on alignment with discussed benefits (e.g., omega-3s for triglycerides, anti-inflammatories for vascular health), and all purchases should be your independent decision after due diligence and consultation with a healthcare professional. No endorsement of efficacy nor any guaranty is stated nor implied; individual results vary.
"The greatest wealth is health."
– Virgil
Interesting Fact 1:
Optimal ancestral cholesterol hovered around 150 mg/dL total (LDL ~100), correlating with minimal ASCVD in hunter-gatherer populations—modern diets push us higher.
"Let food be thy medicine."
– Hippocrates
Overwhelmed by lab chaos?
Ratios like Total/HDL<3 simplify risk—confident control ahead.
Fear heart attack odds?
LDL<100 + lifestyle slows plaque—secure longevity now.
Stuck in metabolic rut?
Target triglycerides<150 via plants—vital energy restored.
Frustrated by "fluffy" LDL hype?
ApoB count trumps size—clearer path forward.
Anxious about family history?
Risk scores + statins protect—family legacy preserved.
Take Action to Live Another Day
Print your lipid panel, calculate Total/HDL (total cholesterol ÷ HDL), and book a clinician chat if >4—act on your dashboard today.
Interesting Fact
HDL function (cholesterol efflux) predicts events better than HDL quantity alone; "lazy" HDL despite high numbers flags hidden risk in 20-30% of cases.
Save Your Family, Friends, and Neighbors
Share your Total/HDL ratio in comments—did lifestyle shift it? Inspire others to check theirs now.
Interesting Fact
Statins reduce major vascular events by 20-25% per 39 mg/dL LDL drop, with benefits compounding over decades—lifetime exposure matters most.
"We are what we repeatedly do. Excellence, then, is not an act, but a habit."
– Aristotle
AI-Selected Cholesterol-Related Products
LiveGood
-
Factor4: A blend of turmeric, fish oil, CoQ10, and garlic designed to combat inflammation, support heart health, reduce oxidative stress, lower blood pressure, and enhance vascular and mitochondrial function for better energy and circulation.
-
Organic Super Reds: Powder with beets, pomegranates, and berries rich in nitrates and antioxidants to boost nitric oxide, improve blood flow, reduce inflammation, support cardiovascular health, and enhance overall energy and immune function.
Summary: LiveGood's Factor4 and Organic Super Reds target cholesterol-related concerns by fighting inflammation and oxidative stress—key drivers of arterial aging—while promoting better blood flow, heart protection, and metabolic balance through natural, affordable supplements that align with lifestyle strategies for optimal LDL/HDL ratios and vascular health.
Isagenix
-
Isagenix Omega-3 Fish Oil: Provides EPA/DHA omega-3s to lower triglycerides, support healthy cholesterol balance, reduce inflammation, and promote cardiovascular wellness.
-
Ionix Supreme: Adaptogenic blend with adaptogens and antioxidants to manage stress, support metabolic health, and indirectly aid lipid profiles via reduced inflammation.
Summary: Isagenix products like Omega-3 Fish Oil and Ionix Supreme offer heart-supportive omega-3s and anti-inflammatory adaptogens that complement cholesterol management by targeting triglycerides, inflammation, and stress-related metabolic factors, helping maintain favorable LDL/HDL ratios as part of a clean, nutrient-dense routine.
Melaleuca
-
Cardio Omega-3: High-potency fish oil with EPA/DHA to improve lipid profiles, lower triglycerides, reduce inflammation, and support arterial health and blood pressure control.
-
Mela-VitaCaps: Multivitamin with antioxidants, CoQ10, and olive extract to combat oxidative stress, enhance heart function, and promote overall cardiovascular resilience.
Summary: Melaleuca's Cardio Omega-3 and Mela-VitaCaps focus on omega-3 delivery and antioxidant defense to optimize cholesterol patterns, mitigate plaque risks from inflammation and oxidation, and bolster heart health—ideal for Americans aiming to refine non-HDL and ratios through targeted, science-backed supplementation.
Young Living
-
OmegaGize3: Triple-action omega-3 with fish oil, orange/lemon oils, and vitamin D3 to support healthy cholesterol levels, reduce inflammation, improve circulation, and enhance cardiovascular and brain health.
-
Inner Defense: Essential oil blend (oregano, thyme, citrus) with immune and antioxidant benefits that may indirectly aid metabolic and inflammatory aspects of heart health.
Summary: Young Living's OmegaGize3 and Inner Defense leverage premium omega-3s and therapeutic oils to address inflammation and oxidative stress tied to poor lipid ratios, promoting cleaner arteries and metabolic terrain for sustained vascular youthfulness.
doTERRA
-
Omega Complex: Fish oil-based EPA/DHA supplement to balance lipids, lower triglycerides, support HDL function, and reduce cardiovascular inflammation.
-
TriEase (or Zendocrine blend): Essential oil complex with anti-inflammatory properties from ginger, fennel, and lemongrass to ease digestive/metabolic stress and complement heart-protective routines.
Summary: doTERRA's Omega Complex and TriEase provide potent omega-3s and aromatic anti-inflammatories to tackle high triglycerides, enhance HDL efficacy, and soothe the insulin-resistant backdrop that amplifies cholesterol risks, empowering proactive artery protection.
Last updated: December 2025.